Clear, Healthy & Confident Skin with Psoriasis Vulgaris Treatment
Psoriasis vulgaris, commonly referred to as psoriasis, is a chronic autoimmune skin condition that causes the rapid buildup of skin cells. It is the most common form of psoriasis and is characterized by patches of thick, red, and scaly skin. The exact cause of psoriasis is not fully understood, but it is believed to involve a combination of genetic and environmental factors. In psoriasis, the immune system mistakenly attacks healthy skin cells, triggering an accelerated growth cycle. Normally, skin cells mature and shed every 28 to 30 days, but in psoriasis, this process takes only 3 to 4 days, resulting in the accumulation of cells on the skin surface.

Symptoms and Causes
Signs & Symptoms Of Psoriasis Vulgaris
Dry, Cracked Skin: The affected skin may be dry, itchy, and may even crack and bleed in severe cases.
Thickened Or Pitted Nails: Psoriasis can affect the nails, causing them to become thickened, discolored, ridged, or pitted. In some cases, the nails may separate from the nail bed.
Itching And Discomfort: Psoriasis can be accompanied by itching and a feeling of discomfort or soreness in the affected areas.
Joint Pain And Swelling: In some individuals, psoriasis can also lead to joint inflammation, causing pain, stiffness, and swelling. This condition is known as psoriatic arthritis and can affect any joint in the body.
Emotional Distress: Psoriasis can have a significant impact on a person’s quality of life and emotional well-being. The visible nature of the condition and the potential for social stigma can lead to feelings of self-consciousness, embarrassment, and depression.


What are the Causes of Psoriasis Vulgaris?
- Genetic Factors: Psoriasis tends to run in families, suggesting a genetic predisposition.
- Immune System Dysfunction: Psoriasis is considered an autoimmune disease, in which the immune system mistakenly attacks healthy cells, including skin cells.
- Infections: Bacterial or viral infections, particularly streptococcal infections, can trigger or worsen psoriasis, especially guttate psoriasis.
- Injury To The Skin: Injuries such as cuts, scrapes, sunburns, or bug bites can cause psoriasis to develop or flare up in affected areas (known as the Koebner phenomenon).
- Medications: Certain medications, such as beta-blockers, lithium, antimalarials, and nonsteroidal anti-inflammatory drugs (NSAIDs), may trigger or worsen psoriasis in some individuals.
- Stress: Emotional stress or physical stress on the body, such as surgery or illness, can be associated with psoriasis flare-ups in some people.
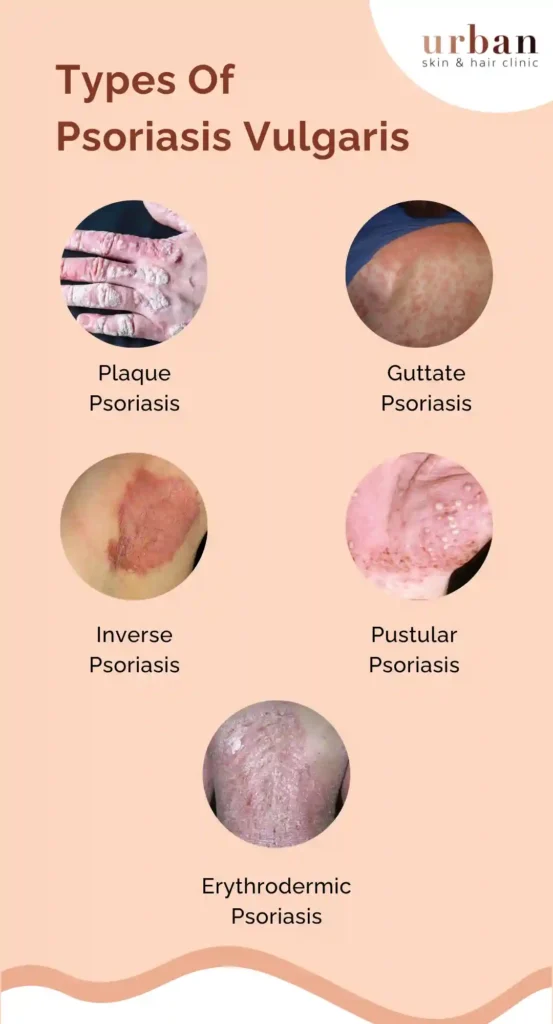
What are the Types of Psoriasis Vulgaris?
- Plaque Psoriasis: This is the most common type of psoriasis, characterized by raised, red patches of skin covered with silvery-white scales. These patches, or plaques, can appear anywhere on the body, but they commonly occur on the elbows, knees, scalp, lower back, and genitals.
- Guttate Psoriasis: This type often develops in childhood or early adulthood and is characterized by small, dot-like lesions on the skin. It is usually triggered by bacterial or viral infections, such as strep throat, and the lesions are typically widespread and appear on the trunk, limbs, and scalp.
- Inverse Psoriasis: This type affects areas where the skin folds or creases, such as the armpits, groin, under the breasts, and in the genital area. Inverse psoriasis appears as smooth, red patches of inflamed skin that may be worsened by friction and sweating.
- Pustular Psoriasis: This type is characterized by the formation of pus-filled blisters (pustules) surrounded by red, inflamed skin. Pustular psoriasis can be localized to certain areas of the body, such as the hands and feet (palmoplantar pustulosis), or it can be generalized and affect larger areas of the body.
- Erythrodermic Psoriasis: This is a rare but severe form of psoriasis that can affect the entire body. It is characterized by widespread redness, intense itching, and peeling of the skin. Erythrodermic psoriasis can be life-threatening and requires immediate medical attention.
Acne - Pimple Treatment Results Before & After











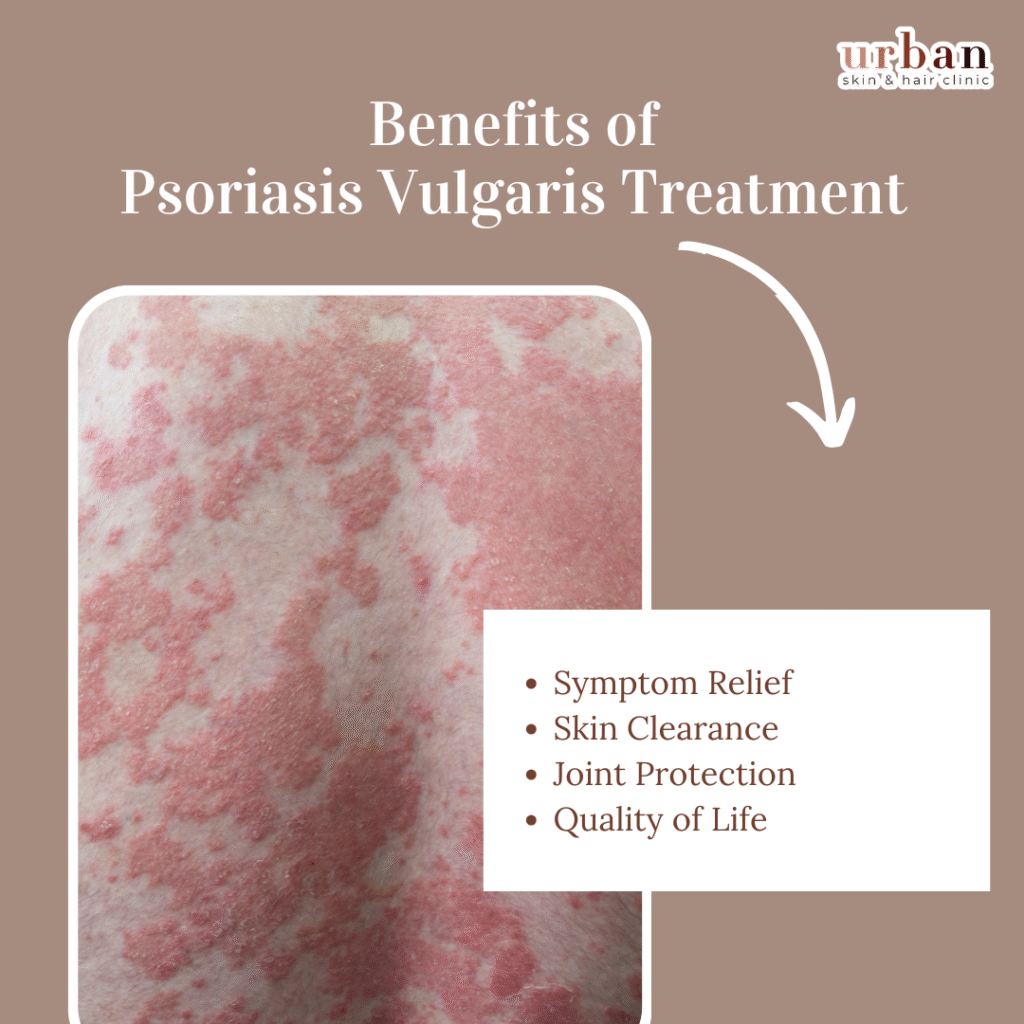
Benefits of Psoriasis Vulgaris Treatment
Psoriasis vulgaris treatment reduces inflamed plaques, scaling, and itching through topical steroids, biologics, or phototherapy.
Symptom Relief
Topical corticosteroids and vitamin D analogs quickly clear plaques, easing discomfort and preventing flare-ups in 70-80% of mild cases.
Skin Clearance
Phototherapy and biologics like IL-17 inhibitors achieve 90% improvement in moderate-severe cases, restoring smoother texture.
Joint Protection
Systemic treatments lower psoriatic arthritis risk by controlling inflammation, improving mobility for affected patients.
Quality of Life
Reduces embarrassment from visible lesions, minimizing depression and enhancing daily confidence with sustained remission.
Popular Treatments for Acne
How To Prevent Psoriasis Vulgaris?
Psoriasis vulgaris cannot be fully prevented due to its genetic basis, but flare-ups can be minimized through trigger avoidance and skin care.
Moisturize Daily
Apply fragrance-free emollients immediately after bathing to lock in moisture and reduce scaling from dry skin.
Manage Stress
Practice yoga, meditation, or therapy regularly, as emotional stress triggers 40% of flares via inflammatory responses.
Healthy Diet
Consume omega-3-rich foods (fish, flaxseeds), fruits, and vegetables while limiting alcohol, smoking, and processed sugars that worsen inflammation.
Sun and Injury Protection
Use sunscreen, avoid sunburns, and cover cuts promptly to prevent Koebner phenomenon where lesions form at injury sites.
Consult a Specialist Today
Many of the techniques for preventing pimples may also be used to cure them. Eating well, avoiding stress, and not popping pimples may help manage zits and reduce their length. If your acne continues despite your best efforts, you may need prescription acne treatment. Consult your dermatologist if you’re uncertain about treatment.
FAQ's
Genetic predisposition combines with immune overactivity, speeding skin cell turnover and causing inflamed, scaly plaques; triggers include stress, infections, or medications.
No, it’s an autoimmune condition, not infectious—scales result from rapid cell growth, not bacteria or viruses.
Yes, it links to psoriatic arthritis (30% risk), cardiovascular issues, and metabolic syndrome from chronic inflammation.
No cure exists, but treatments like topicals, biologics, and phototherapy achieve 80-90% clearance and long remissions.
Stress, smoking, alcohol, skin injury (Koebner phenomenon), cold weather, or infections provoke outbreaks in genetically susceptible individuals.